PHE & Healthcare: Why Health Plan Executives Need to Update Reimbursement Policies Post PHE
With the expiration of the COVID-19 national public health emergency (PHE) on May 11, healthcare executives need to prioritize updating payment policies and procedures to reflect regulatory changes or risk billing errors that may negatively impact member and provider relations.
The decision by the White House on January 30 to end the PHE, as the New York Times aptly put it, carries “symbolic weight and real-world consequences.” Symbolically, the pronouncement signaled that the worst of the pandemic is likely behind us. As for real-world implications, the move meant that healthcare coverage changes will influence how healthcare can be accessed and reimbursed by payers for both members and healthcare providers.
During the pandemic, health plans loosened a wide range of policies, citing exceptions related to the PHE. Some healthcare plans, for example, turned off National Correct Coding Initiative (NCCI) edits for specific services and/or providers. The end of the PHE allows health plans to reinstate former payment integrity policies. With the federal government rescinding financial support for vaccines and repealing policies and regulations that enabled shifts to remote care and covered select COVID-19 costs, healthcare payers now can reassess current reimbursement practices. Upon the conclusion of the PHE, a thorough investigation of formerly waived policies and regulations is required to assure accurate claims reimbursement.
Challenges for Health Plan Executives
The financial pressure to avoid overpayments weighs heavily on health plan executives as claims management systems must be reconfigured to align with new or reinstated policies affected by the end of PHE. During this transitional period, it is critical that health plans review, make the necessary modifications, and communicate changes to members and providers to avoid abrasion.
Health plan operations leadership must move quickly to ensure that billing policies and procedures adhere to the new federal and state regulations and those changes are clearly communicated to the claims system configuration teams responsible for the configuration updates.
Here are a few key changes that must be addressed to prevent improper claims processing:
- During the PHE, federal funding for the vaccine made it unnecessary for providers to bill for reimbursement for vaccines. However, going forward, providers must bill for the COVID-19 vaccine in addition to the vaccine administration.
- For most private health insurers, member cost sharing will be impacted by out-of-network administration of the COVID-19 vaccination, while there will be a continuation of no cost sharing for in-network providers.
- There will no longer be mandatory coverage for over the counter and laboratory-based COVID-19 PCR and antigen tests. Medicare will continue to provide no cost sharing for physician ordered testing, while private health insurers may choose to continue coverage for tests, institute cost sharing and require prior authorization.
- As a requirement of the American Rescue Plan Act of 2021 (ARPA), States must continue to provide Medicaid and CHIP coverage for COVID-19 vaccinations, testing, and treatments without cost sharing through September 30, 2024.
Health plans also need to consider revising telehealth policies to avoid overspending during this transition period, while taking into consideration the ease of access to care offered through telehealth, and the resulting potential for member pushback and provider abrasion.
Vaccinations and telehealth are just a few of the obvious areas, not to mention those with more complex requirements, such as behavioral health and substance use, lab testing and presumptive urine drug screens, physical therapy, early pharmacy refills, early DME disbursement, and extended skilled nursing facilities (SNF) / home health length of stay. Each of these areas needs to be addressed for reduced risk and managed costs.
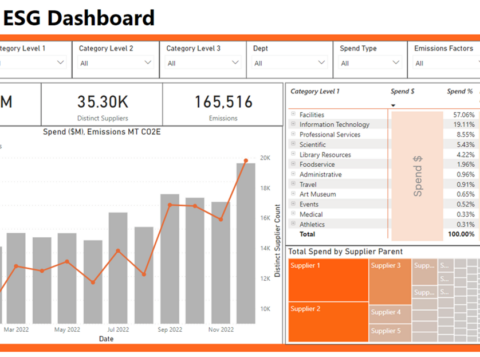
Updating policies and procedures requires health plan executives to closely examine a wide spectrum of payment processes, contract management systems, and utilization management programs. CMS guidelines are a helpful resource, but there remains a heavy lift for most health plans’ contracting and configuration departments. We expect more MCOs to partner with consulting firms such as AArete to assure timely compliance of policies and procedures to mitigate risk and control costs.
With the end of the PHE rapidly approaching, urgency is required to update reimbursement policies and procedures to assure proper claims reimbursement, enabling healthcare providers to deliver uninterrupted care for patient satisfaction and improved health outcomes.
About AArete’s Payment Intelligence®
The setup of a payer’s system for processing claims impacts the accuracy of payments. Several service providers offer continuous payment precision services, but AArete’s Payment Intelligence® stands out by detecting, comprehending, retrieving, and correcting improper payments to prevent future occurrences. Adjustments made in the system to enhance payment precision invariably result in enduring enhancements in the profitability of the client.