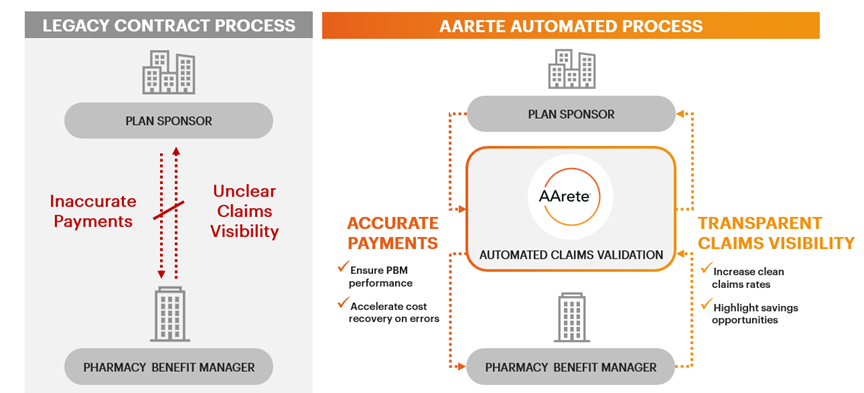
Pharmacy Benefit Manager (PBM) contracts represent one of the largest and most complex expenditures for healthcare payers, often exceeding $100 million monthly. PBMs significantly influence critical decisions, from drug pricing and rebate structures to patient cost-sharing and formulary design, often creating challenges in ensuring alignment with a payer’s strategic, financial and member-centric objectives.
With federal and state reforms driving higher audit standards, growing demand for transparency, payers need more robust oversight to mitigate risks and foster long-term value. Partnering with an experienced third-party consultancy brings the expertise, objectivity, and innovative strategies required to navigate this intricate landscape, optimize member and provider experiences, and deliver sustainable financial and operational success.
Our Approach
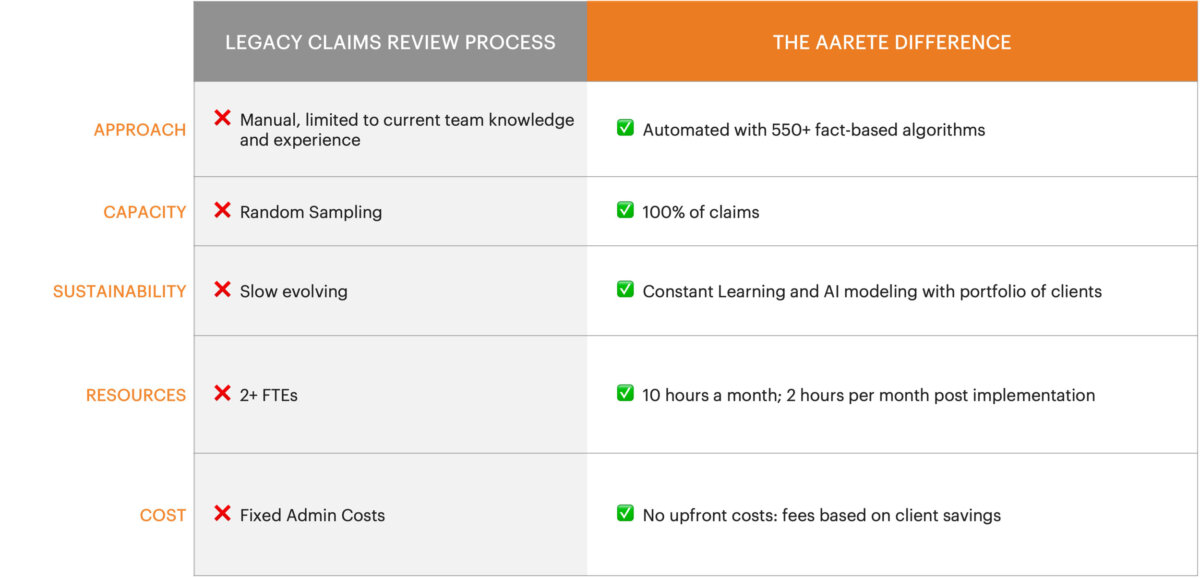
AArete works with health plans to automate the analysis of 100% of PBM claims after each claim adjudication cycle, identifying and correcting claim discrepancies, saving health plans 0.5%-3% annually while gaining more financial control. We are unbiased and committed to the mission with a dedicated focus on achieving client-specific goals.
Benefits
Transparency & Control
- Visibility in real-time with 550+ algorithms
- Claim errors identified for resolution at any point in time
- Empowers health plan with more information and greater transparency
Financial Control
- Provides an invoice validation tool, better financial predictability and more control
Enhanced Oversight
- Continuous claims monitoring for contract compliance
- Validate benefit administration accuracy
- Proactive approach instead of contentious PBM audits
Lower Costs
- Automated process eliminates health plan manual processes
- Claim reversals and recoveries achieved within plan year
- Root cause analysis and corrective action for cost avoidance
Why AArete?
Choose AArete for 100% risk-free cost savings with minimal lift from your team, leveraging conflict-free, PBM-agnostic expertise and AI-driven insights to optimize performance and deliver lasting value.

Free of Conflicts
Unbiased third-party validation of PBM performance

Works With Any PBM
Maximize pharmacy contract performance works with any PBM

Tech-Enabled Rx Analysis
Validation of automated claims against complex custom PBM contracts, plan designs and formularies