AArete Develops Customized Cost/Quality Matrix to Help Regional Health Plan Optimize its Primary Care Network
Situation
A Medicaid Managed Care Organization’s (MCO) network of Primary Care Providers (PCP) included a substantial portion of low-quality, high-cost physicians. The MCO reported that the network performance was increasing overall costs and negatively impacting member experience. The organization approached AArete to optimize the PCP network by increasing the proportion of high-quality, low-cost PCPs.
Approach
In order to develop a custom predictive model, AArete worked closely with the client to understand how they defined player success. From there, we determined the appropriate way to translate this definition into a variable to be used in the model. Prior to initiating our modeling process, AArete compiled a comprehensive data warehouse of quantitative data, which represented player attributes and performance, and qualitative data, which represented external factors like player behavior and other elements that could not be captured in the quantitative data. Once our team compiled the warehouse, we applied cutting edge machine learning techniques, leveraging our distributed computing environment to test iterative models. Ultimately, our model was able to confidently predict a respective player’s success potential based on the client’s unique definition.
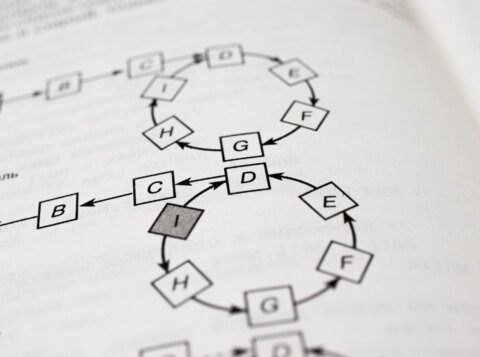
Using insights from stakeholder interviews and plan analytics, AArete identified key HEDIS measures for the plan and segmented the provider network by cost, risk accountability, provider specialty, high-cost member impact, and other variables. With this information, we created customized Quality/Cost matrix and membership-based, geo-spatial models to ensure identified opportunities did not limit access to care. These models aided in generating implementation strategies, which ranged from terminating high-cost, low quality providers to developing value-based contracting arrangements for certain providers. We proposed multiple implementation plans to allow for flexibility and varying regulatory factors, while taking local relationships into account.
Results
The selected implementation strategies reduced expenses by 3% in the pilot market, with potential savings of 6% to 10% in the secondary market – a total savings opportunity of more than $3 million for the health plan. Additionally, the PCP network optimization efforts will improve member experience by holding long-term impact on provider performance and quality, ultimately improving member experience.