4 Proven Strategies Medicaid Leaders Can Implement to Enhance Member Care, Lower Costs in 2024
This is an AArete Healthcare Payer insight
With 2024 still in its infancy, Medicaid health plan leaders have an ideal opportunity to start the new year fresh by accelerating the integration of innovative technology to increase productivity, safeguard operating margins, and enhance member care.
Technology will play an increasing role in protecting operating margins because enrollment in many Medicaid plans is expected to decline this year. KFF estimates that Medicaid membership will decrease by 8.6% in fiscal year 2024.

Cutting-edge digital tools, including generative artificial intelligence (AI), machine learning (ML), and robotic process automation (RPA), hold enormous power to boost the productivity of an organization’s most important resource: its people. The growing sophistication of these technologies allows leaders to take a holistic approach to deliver sustainable improvements in member service and organizational cost reductions – rather than one-time layoffs and/or budget cuts.
Here are four core strategies plan leaders can implement to generate long-term value, better manage the cost of care, and help improve health outcomes for their members:
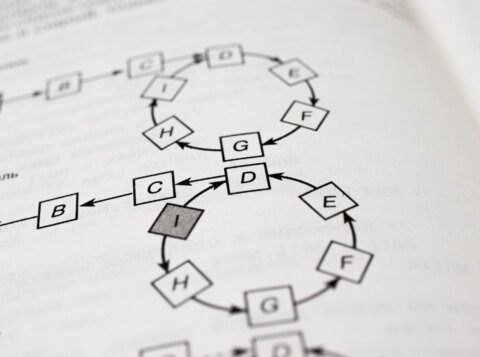
1. Automate processes to improve operational efficiency
Use the start of the new year to conduct a strategic review of operations to identify opportunities where technology can quickly increase efficiency and enhance team member productivity. For example, look at how regularly
scheduled management reports are compiled. In our experience, we have found that different markets use different processes – many of them manually intensive – to generate the same report.
Generative AI, ML, and RPA technologies can be deployed to automate a wide range of general and administrative (GA) and member support tasks. These tools have an immediate, positive, cascading impact on your organization. They can be a key enabler to optimizing workflows so your team spends less time on GA duties and more time finding creative, cost-efficient ways to better serve members.
2. Integrate AI to enhance member experience
Redetermination has changed the member mix at nearly every Medicaid plan and resulted in an increased proportion of higher-acuity members. The good news is that Medicaid populations at most plans have normalized and likely more closely resemble a pre-pandemic member mix.
The difference from pre-pandemic is the development of AI-powered applications that can help organizations provide better service to members. The technology can, for instance, supercharge predictive analytics to identify high-risk members. That data allows your team to proactively engage with those members and help them receive timely care to improve their health and avoid more high-cost claims. It is a win for everyone. Members are happier because they potentially avoid severe health issues. Plans benefit because healthcare costs are lower, which also eases the financial strain on state and federal government Medicaid programs.
3. Optimize prior authorization processes
Prior authorization has been a key focus for health plans since December 2022 when the Centers for Medicare & Medicaid Services (CMS) proposed new regulations that included rules to facilitate approvals. With Medicaid populations stabilizing as redetermination moves to a steady state, plan leaders can now better understand the healthcare status and future needs of their member population.
Decision-makers can review prior authorization processes and approval/denial rates to find ways to lower authorization volume for certain treatments and drugs. Optimizing the process can help decrease administrative costs and elevate member satisfaction because care can be delivered quickly.
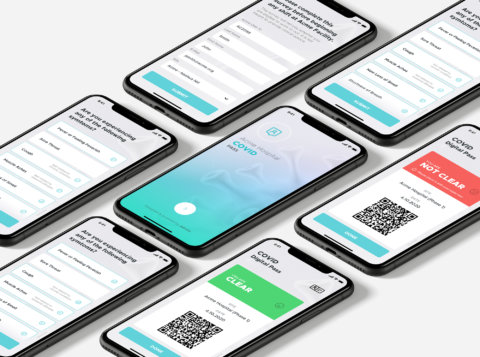
4. Review vendor contracts
As organizations juggle a growing number of projects, it is easy for leaders and team members to get overwhelmed, and some areas of the business receive less attention than others. In our work with plans across the country, we have found that reviewing provider and vendor contracts often ranks low on the list of priorities.
That is a big mistake. Do not underestimate the potential cost savings your organization can realize by reviewing contracts to generate mutually beneficial pricing. Today’s AI-enabled document management technology can facilitate the review and analysis of contracts to help determine if you are receiving the best services at optimal prices. Work with your care providers to find ways to fine-tune value-based care contracts that lower costs and provide superior member care. As a recognized leader in healthcare payer consulting, AArete can provide you with up-to-date market intelligence so you can make informed decisions on the cost and value of the services your plan is purchasing.
At AArete, we believe 2024 will be a pivotal year in validating how investments in AI-powered technology will fundamentally transform the way healthcare is delivered while helping plan leaders become better stewards of the state and federal funds that support U.S. Medicaid programs.
If you are searching for cost-effective, practical solutions to advance your organization’s technology infrastructure and improve service to your Medicaid members, please contact us. Our team of healthcare and technology experts are ready to help.
Learn more about AArete’s Healthcare Payer Consulting and Practical AI Solutions.