An Opportunity for Provider Status

The past several decades has been the passage of “provider status” laws for pharmacists in many states. While the specifics vary from state to state, the general intent behind this legislation is to give patients increased access to some of the oft-underutilized services that pharmacists can provide. People place significant trust in their pharmacists for a host of reasons, including ease of accessibility and their frequent contact with them. Now, as the COVID-19 pandemic rages on, pharmacists are needed to help relieve some of the burden on highly strained health care providers on the front lines. The good news is, they’re well equipped to do so, though regulatory obstacles and some issues around payment models for their services are currently preventing them from expanding their services.
Two test cases
The concept behind pharmacist provider status goes back more than 20 years. In one instance, known as the Asheville Project, the City of Asheville, N.C., launched a program in 1997 to provide education and oversight to municipal employees with chronic health problems, including diabetes. As part of this program, community pharmacists worked with the employees to help them use their medications properly. This particular patient-centered program was payer-driven and provided a significant return on investment by lowering total health care costs, reducing sick days and keeping these employees from the emergency room visits due to diabetic complications. Louisiana, Maryland, Texas and West Virginia are among the states that have since adopted policies giving pharmacists provider status for diabetes management.
Another critical area where pharmacists have become providers is vaccination. In 1996, the American Pharmacists Association established the Centers for Disease Control and Prevention (CDC) -endorsed Pharmacy-Based Immunization Delivery program, which teaches pharmacists how to provide vaccine education and administration. By 2009, all 50 states permitted pharmacists to administer vaccinations, albeit with varying education or certification requirements and, in some states, limitations around the types of vaccinations pharmacists can administer. The handful of “holdout” states were motivated to grant this status by the 2009 H1N1 pandemic.
Untapped opportunities
Recent pharmacy college graduates receive even more training than previous generations, with many opting to specialize in areas like cardiology, infectious disease, hematology/oncology, and pediatric or geriatric care. This specialized knowledge can be applied in their daily work when they are permitted to advise, educate and even prescribe drugs rather than simply filling prescriptions, guarding against problematic drug interactions and consulting with patients about any new or changed medications.
Many pharmacists work in an informal advisory or educational capacity, frequently recommending over-the-counter solutions to help alleviate a patient’s symptoms or suggesting they see their general practitioner when symptoms suggest a serious condition. When empowered to provide services at a higher level, they can work in more of a clinical capacity by providing comprehensive medication reviews; smoking and tobacco cessation counseling; diabetes education; and other value-added services.
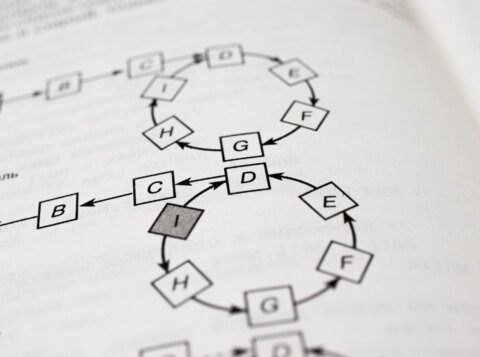
In the case of certain ailments such as asthma or diabetes, when allowed to prescribe medications, pharmacists have been able to get patients on a path to recovery sooner than if the patient had had to schedule an appointment with a traditional provider. Some states allow them to do so for certain classes or types of drugs — for example, pharmacists in Florida can prescribe some cough and cold medications, while all states now allow pharmacists to dispense naloxone without a prescription. Under current collaborative practice agreements, pharmacists can modify or even switch out drugs under a physician’s oversight; a more independent, time-sensitive approach to this capability that empowers pharmacists to do so without this oversight could be a part of the future.
Increasing prescriptive authority might cause some physicians’ resistance, questions about liability, or possible increases in malpractice premiums. The small possibility of a negative outcome notwithstanding, the upside is tremendous. People already know that pharmacists have expertise around medication, and they are also more readily available than traditional providers. Another important consideration is that many patients see multiple doctors whose care may not be well coordinated; most only see one pharmacist, however, and that resource can view all of a patient’s information and also monitor how well a patient is doing around refilling their prescriptions. As electronic prescribing and other technologies that support pharmacy technicians taking on more of the pharmacist’s traditional dispensing duties become more commonplace, pharmacists can practice at the top of their license by serving their communities as additional care providers.
Urgent action needed
In a sense, the pharmacist provider status movement harkens back to an earlier time, when every community had a druggist who could be depended upon to field questions about aches, pains and sniffles and suggest a remedy. We are now in a “back to the future” moment in which pharmacists can once again take on this elevated role as providers — a role that benefits patients, traditional providers and pharmacists themselves. Doing so on a more widespread basis will require states to act, though payment models must also be established to ensure that pharmacists receive payment for provider services. Better still would be national legislation for provider status, which would open the door for pharmacists to provide services to Medicare patients and establish a Medicare fee schedule.
We are seeing how the current pandemic is bringing new urgency to health care advancements, as demonstrated by how quickly many systems have added telehealth capabilities during this pandemic after years of delays — and now, allowing pharmacists to order and administer COVID-19 testing. This same urgency should be applied to finding ways to grant pharmacists provider status in order to open the door for medication therapy experts to expand their services. Steady progress has been made, but the time is here for a step change to help alleviate some of the pressure the health delivery system faces.
This article was originally published in Chain Drug Review.