Behavioral Health Care Management Program Optimized by Targeting Members with High Impact and Engagement
This is an AArete Healthcare Payer Insight
Situation
A leading Medicare Payer was looking to improve prioritization for Behavioral Health Care Management and recommendations on program staffing for a cohort, with $269M of annual spend.
Approach
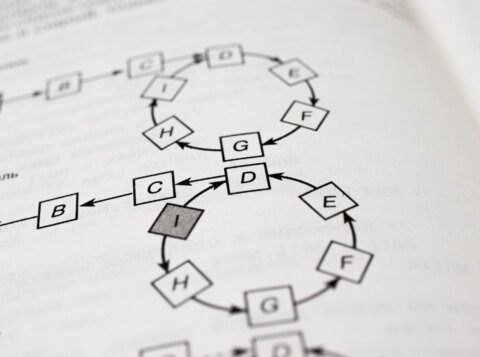
AArete prioritized members based on targeting their impact and engagement. The impact showed that the spend profile and diagnosis were highly modifiable with high savings potential, while the engagement reflected the members’ likelihood to engage with care managers and improve behavior.
AArete identified initial vulnerable populations, and rising risk populations with predictive analytics, and showed who was most likely to engage and improve health outcomes. AArete also designed interventions and developed program staffing.
Results
As a result, the client has established feedback monitoring and has set up a repeatable process. They are also estimated to achieve:
• 35% increased member engagement
• 8-13% savings (cost avoidance) on cohort spend annually
Learn more about AArete’s Profitability Improvement Solutions