Health Plan’s Prior Authorization Strategy Created, $28M in Savings Identified
This is an AArete Healthcare Payer insight
Situation:
A health plan engaged AArete to provide an objective assessment of the prior authorization process, costs and compliance with clinical policy, and regulatory requirements.
The plan delegated prior authorizations to the PBM for all lines of business, and was interested in assessing the effectiveness of the PA criteria, UM controls and had been considering insourcing the process.
Approach:
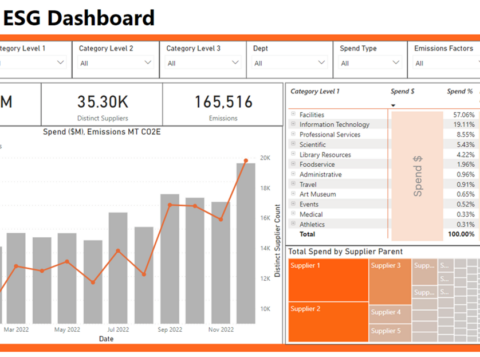
AArete collected the most current 12 months of prior authorization and claims data. PA volume, approval, denial, and appeal rates were analyzed by drug, intake channel, pharmacy, and provider.
Approvals and denials were reviewed against clinical policy criteria and industry best practices. The cost per PA was determined based on total PA cases and total PBM administrative fees.
Results:
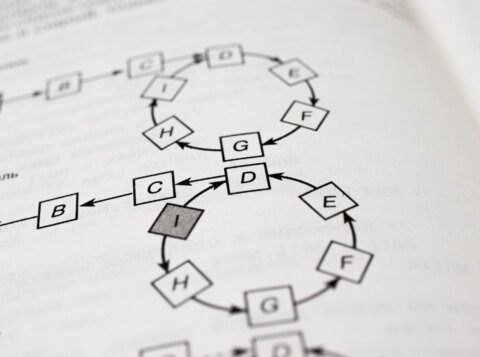
The review uncovered several improvement opportunities with the clinical criteria administered by the PBM, formulary changes and removal of some drugs from the PA list which could drive as much as $28M in savings.
A PA strategy and roadmap was developed to drive improvements and assess the feasibility and ROI of insourcing some or all PA components.
Learn more about AArete’s Pharmacy Solutions