Transforming the Payer-Provider Relationship in the Era of Medicare Advantage Growth
This is an AArete Healthcare Payer & Provider insight
Rebuilding trust through personal connection
There’s currently a lot of mistrust between payers and providers. Historically, providers have been incentivized to focus on the elements of member interactions that are reimbursable. Payers, meanwhile, have been focused on monitoring practices like overbilling, fraud, and abuse. Unilateral decisions have been made on both sides that affected the flow of money, leading to hard feelings.
Rebuilding trust and overcoming skepticism from both parties comes by establishing credibility, than demonstrating real results. In working with clients in the past, we’ve found that bringing together care coordination personnel from both the payer and provider camps, such as medical directors, is an effective way to break down defenses and bring empathy to discussions. By resetting the payer/provider relationship and finding common ground, it’s often possible to build a sense of collaboration.
Reducing administrative burdens
Both payers and providers are dealing with ongoing workforce shortages, which creates administrative challenges and leads to a shortage of institutional knowledge. Some keys to reducing these burdens include delegation of responsibilities, streamlining benefits, and maintaining open lines of communication about challenges. By simplifying administrative processes, both parties can free up resources to focus on patient care and improve overall efficiency.
Using data to drive results
Payers and providers both care about delivering the best possible care for patients, but they tend to talk about quality in different ways. Engaging in open, transparent discussions can help payers and providers understand each other’s perspectives and work toward shared objectives.
Data is the universal language of business, and using it as a starting point can normalize a conversation between the two parties and take the emotion out. As payers collect data, they need to share it with providers in an actionable way that creates strong insights and value. Payers should work to help providers understand the importance of, and logic behind, the CMS star rating system that is used to assess a provider’s quality of care. This can incentivize providers to align their practices toward high-quality, timely care — not just to improve their star rating, but also to drive improved patient results.
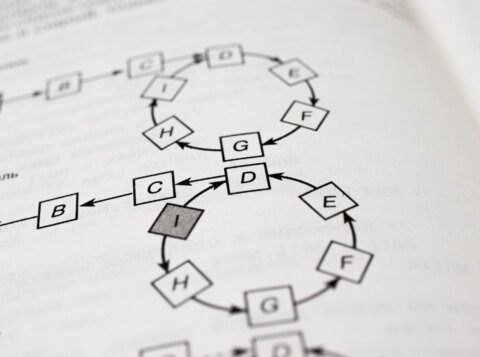
Building a solid governance structure
A solid payer-provider governance structure is essential for supporting effective communication and collaboration. Payers and providers can foster collaboration by setting shared goals, establishing agreed-upon metrics, and putting workable processes in place to resolve concerns from both sides. Effective governance will help in improving care coordination and easing the administrative burden on providers, allowing them to focus more on patient care.
Change that can start today
Ongoing shifts in health care — the movement toward outcome-based care and away from a fee-for-service model, as well as the growth of Medicare Advantage enrollments — can serve as an overdue catalyst for payers and providers to reexamine their historical relationship and strive for something better.
By establishing new practices —open communication, the sharing of actionable data, effective governance structures, and a collaborative attitude focused on the welfare of the patient — payers and providers can pave the way for a more productive, patient-centered future. There’s no need to wait, either — today’s the best day to start.
To hear more of the thoughts we recently shared with Value-Based Insights, listen to the full interview on Soundcloud, YouTube or Spotify.